Dr Lee Featured in Goop
 In a recent appointment, gynecologist Bruce Lee, MD, saw a woman who looked eight months pregnant. She wasn’t. But the benign tumors in her uterus had grown so large that it looked as if she might be. She was seeing Lee that day to get those tumors, called uterine fibroids, treated for the first time.
In a recent appointment, gynecologist Bruce Lee, MD, saw a woman who looked eight months pregnant. She wasn’t. But the benign tumors in her uterus had grown so large that it looked as if she might be. She was seeing Lee that day to get those tumors, called uterine fibroids, treated for the first time.
The reason this patient had waited so long to get help, says Lee, is because the standard treatment for fibroids is a hysterectomy: a full removal of the uterus from the body. The patient didn’t want a hysterectomy, so she hadn’t received any treatment at all. In the meantime, her fibroids grew larger, and her symptoms got worse.
While the size of this patient’s fibroids was particularly astounding, Lee says her case is not unique. An estimated 12 million women in the United States alone, including a disproportionate number of black women, have symptomatic fibroids. The total number of hysterectomies per year (including those for reasons other than fibroid treatment) is about 400,000, according to a 2015 study published in the American Journal of Obstetrics and Gynecology. The same study states that a hysterectomy is used inappropriately in an estimated 17 to 70 percent of total procedures. Which means that of the small fraction of women who do receive treatment for fibroids, many are overtreated with a serious surgical procedure that involves losing an organ.
According to Lee, there are several issues here. The first is lack of funding for women’s health research. The second is a lack of physician and patient education about fibroids. And the third—where Lee thinks he can make the most impact—is a lack of awareness of and access to treatments other than hysterectomy.
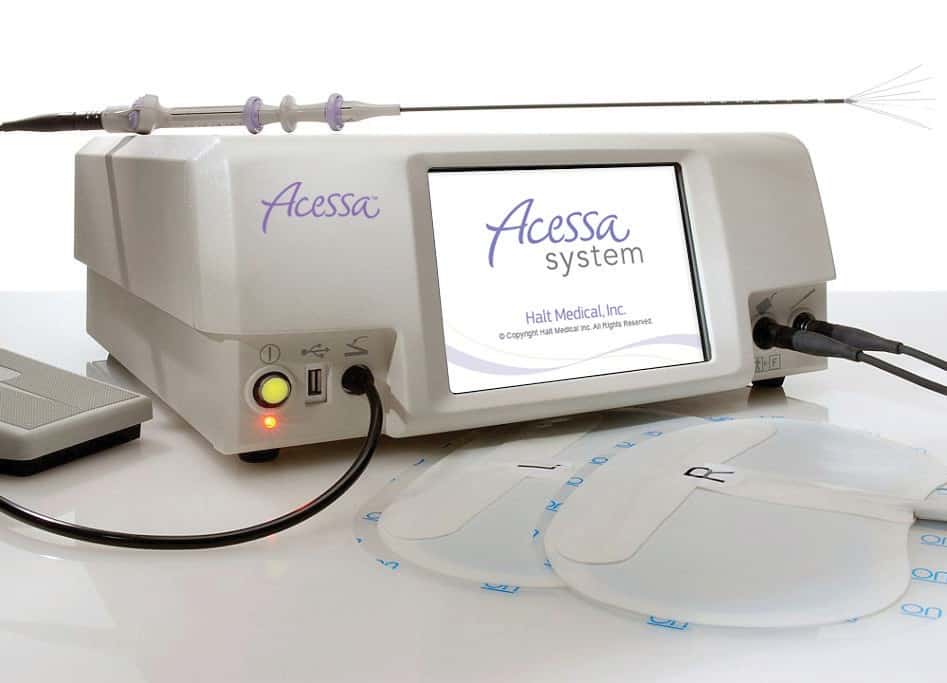
The truth is: If you have fibroids, you do have less-invasive options. Lee is the inventor of a procedure called Acessa, an FDA-approved treatment for fibroids that he’s been performing and training other physicians in for twenty years. It involves a small incision, a needle, some heat, and very little pain or recovery time. While we still have a lot of work ahead of us to make women’s health a priority in medical research and practice, Acessa is a huge step forward for those suffering with fibroids who have been told a hysterectomy is their only way out.
Q: What are uterine fibroids? What do the symptoms typically look like?
A: I am a gynecologist, and I’ve taken a special interest in a common tumor called uterine fibroids. The medical term is uterine leiomyomata. Fibroids are the most common tumors found in women in their reproductive years. They can arise from the time women start their menstrual cycles—although fibroids in teenage women are relatively uncommon—to the time of menopause. By age fifty, an estimated 70 percent of white women have fibroids; in black women, it’s over 80 percent. Black women, unfortunately, have more frequent and numerous fibroids, and they often grow more aggressively and cause more symptoms.
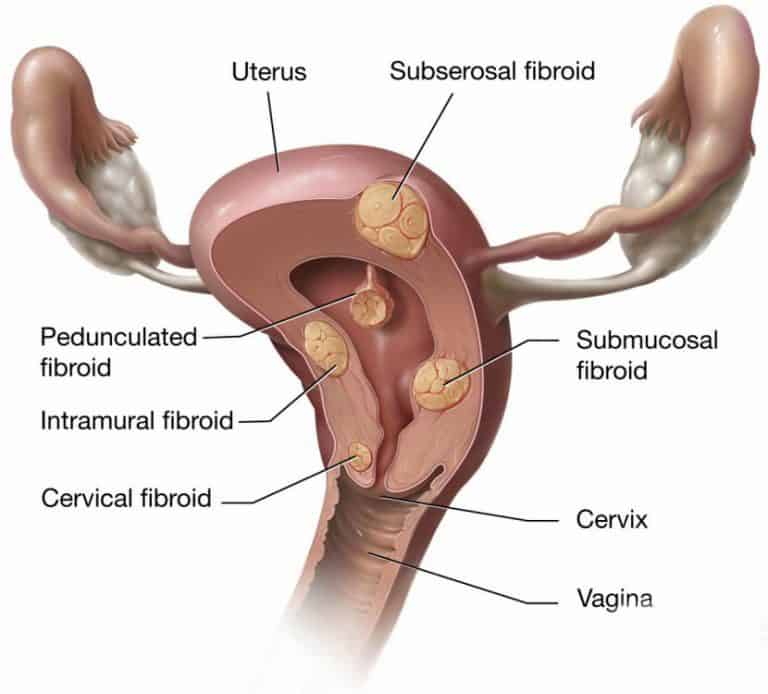
Of women who have these tumors, 40 to 50 percent have symptoms such as heavy menstrual bleeding, worsening menstrual and pelvic pain, and something we call bulk symptoms: pressure on the abdomen, pelvis, bladder, and rectum that’s associated with the size of the tumors. Bulk symptoms can also include pain with intercourse, high urinary frequency, or the appearance of a distended abdomen. For example, if their fibroids are very large, women may look like they are pregnant even though they aren’t.

For diagnosis, a gynecologist can palpate for fibroids with a very careful pelvic exam, but fibroids aren’t easy to feel unless they’ve started to grow larger. If the gynecologist notices that the uterus is irregular in shape or a little larger than it should be, then they might be tipped off that they need to do an ultrasound or MRI to visualize the muscle wall of the uterus. Once you’re using those tools, fibroids are usually pretty visible.
Despite the fact that fibroids are very, very common, they’re not paid enough attention in medical research and practice. Many women who have fibroids don’t get them diagnosed until they’ve had them a long time. Options for treatment are limited: Fibroids are the most common reason women have a hysterectomy.
Q: Where do fibroids come from?
A: Uterine fibroids have been around as long as we have. The ancient Greeks wrote about uterine fibroids. We find uterine fibroids in Egyptian mummies. They don’t arise because of any particular behavior or definable hormone imbalance or dietary issue or environmental influence. What happens biologically is a stem cell called a pluripotent mesenchymal cell goes haywire and becomes a fibroid cell instead of a uterine one. That one fibroid cell will replicate itself over and over and over again until it becomes a fibroid tumor.
It’s common for women to have quite a few fibroids. Actually, it’s uncommon for women who have fibroids to have just one. I’ve treated as many as eighty-six fibroids in a single patient—though a number that high is uncommon.

Q: How can people with fibroids manage their symptoms?
A: Some symptoms are manageable. Some are not. For example, if the fibroid is causing the uterus to put pressure on the bladder, and we get bladder dysfunction such that it doesn’t empty well anymore and you have to go more frequently, we cannot stop symptoms with just medication or behavioral changes.
If a fibroid is causing pain—say, if it presses on the side of the pelvis and causes nerve pain down the legs or into the hips—that can be ameliorated with anti-inflammatories. If fibroids cause pain with intercourse, same thing. But in both of those cases, that doesn’t really take care of the root problem.
If heavy menstrual bleeding is a symptom, we can work on that. There are medications that can decrease the bleeding a little bit. Tranexamic acid can decrease menstrual bleeding by about 20 percent, and nonsteroidal anti-inflammatories, like ibuprofen and naproxen sodium, can help as well. A progestin-only IUD can significantly decrease heavy menstrual bleeding for a while, as can a standard oral contraceptive pill. The pill can also help as decrease cramping. If someone’s fibroids continue to grow, however, eventually these symptoms will return.
Q: Can fibroids cause complications for pregnancy and childbirth?
A: They can. It depends on where in the uterus the fibroids are and how large they are. That may impact pregnancy and childbirth at one of several points:
Fertilization: Especially large fibroids can cause so much pressure that they can compromise the function of the fallopian tubes, which can impact fertilization.
Implantation: The closer fibroids are to the uterine cavity—where embryo implantation would happen—the more likely it is that the implantation process may be disrupted. That could result in miscarriages.
Preterm labor: If someone with larger fibroids does get pregnant, it is possible that they will experience complications such as preterm labor—labor that starts before the baby has reached full term. This can happen as early as sixteen to twenty weeks into a pregnancy. Those pregnancies are commonly lost.
Malpresentation: Fibroids can cause malpresentation, meaning that the baby doesn’t present vertex (head down). Instead they might present breech (head up) or even transverse if the fibroids inhibit the normal descent of the baby through the birth canal.
Postpartum hemorrhage: Large and bulky fibroids can contribute to postpartum hemorrhage. Normally, as soon as the baby is delivered and afterbirth is delivered, the uterus contracts quickly to stop the bleeding. That’s part of its job. (It’s also one of the mechanisms by which the flow of a menstrual period ceases.) But large fibroids can inhibit that process, and bleeding continues—sometimes to a degree that’s extremely urgent and life-threatening to the mother.
Q: When is treatment necessary? What does treatment typically look like?
 A: About half of all patients who have uterine fibroids never develop symptoms. If the fibroids remain small and symptoms do not appear, treatment isn’t necessary, and in those cases the fibroids can be monitored.
A: About half of all patients who have uterine fibroids never develop symptoms. If the fibroids remain small and symptoms do not appear, treatment isn’t necessary, and in those cases the fibroids can be monitored.
However, there are so many women with uterine fibroids right now who need help but are not getting it. The reason they’re not getting help is largely because they didn’t or don’t like the options that they’ve been given. When a woman is diagnosed with fibroids and recommended treatment, the most common answer they get is that they should have their uterus removed. A hysterectomy is a major surgery—recovery time is six weeks or more—and very few people want to have an organ removed if they don’t absolutely have to.
In some cases, women are offered myomectomy, which means cutting out the tumors from the wall of the uterus one by one and then repairing the wall as best as possible. This is still a major surgery with a lot of recovery time, and the uterus might not tolerate the treatment very well. When you cut into the uterus, you’re damaging the muscle wall and then trying your best to repair and help it recover. You can only do that so many times before uterine function becomes compromised. If you have a myomectomy and then become pregnant, most of the time, childbirth will require a Cesarean section to avoid the possibility of the uterus rupturing and opening up during the course of labor.
Q: What is Acessa, and how is it different from typical fibroid treatment?
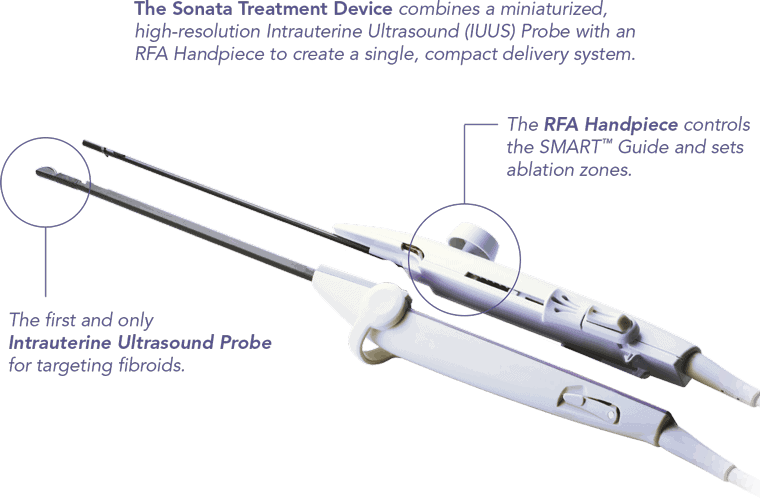
 A: There’s a less common procedure, which I developed and have been practicing for twenty years, called Acessa. With Acessa, we don’t have to remove anything. Using a specialized ultrasound device (which allows us to find up to twice as many fibroids as a pre-op ultrasound and 50 percent more than an MRI) as a guide, we place a needle into each fibroid and do something we call radiofrequency ablation, meaning we treat the fibroid with heat. We can control that heat to restrict it to just the fibroid so that it doesn’t damage normal tissue. The heat breaks down the fibroid into small fragments of protein so that it’s no longer an assembled tumor. It’s like if you have a Lego model of an airplane and you break down that airplane into its Lego pieces—it’s not an airplane anymore, just building blocks.
A: There’s a less common procedure, which I developed and have been practicing for twenty years, called Acessa. With Acessa, we don’t have to remove anything. Using a specialized ultrasound device (which allows us to find up to twice as many fibroids as a pre-op ultrasound and 50 percent more than an MRI) as a guide, we place a needle into each fibroid and do something we call radiofrequency ablation, meaning we treat the fibroid with heat. We can control that heat to restrict it to just the fibroid so that it doesn’t damage normal tissue. The heat breaks down the fibroid into small fragments of protein so that it’s no longer an assembled tumor. It’s like if you have a Lego model of an airplane and you break down that airplane into its Lego pieces—it’s not an airplane anymore, just building blocks.
Those protein fragments can now be reabsorbed by the surrounding uterine muscle. As the body reabsorbs the broken-down protein, the fibroids decrease in size. Small and medium fibroids generally disappear entirely within several months following the procedure. Very large fibroids—the size of a softball on up—generally decrease in volume by about 60 or 80 percent, although it is possible for them to completely disappear as well.
Also, as soon as we treat the fibroid, it’s no longer a biologically active tumor as fibroids normally are, so it can’t act out the biological processes that would cause heavy menstrual bleeding or some of the processes that increase pain. So we get symptom relief fairly quickly.
We don’t use any narcotics afterward for pain control—just nonsteroidal anti-inflammatories, like ibuprofen, plus a heating pad.
The FDA has not cleared Acessa for women who wish to become pregnant because we haven’t reported any data to the FDA yet on pregnancy outcomes. (There is no negative data, though.) In my practice I’ve seen women who have been infertile become able to conceive after we’ve treated their fibroids. Because we are not cutting into the wall of the uterus and causing damage, I allow my patients to deliver vaginally.
We can do this with just one skin puncture. It can often be done in a single procedure, although for some very large and more difficult cases, treatment may be broken up into stages.
The post Why Uterine Fibroids Are the Most Commonly Overlooked Tumors in Women appeared first on Dr. Bruce B. Lee.
